HOW IS SUI TREATED?
 Lifestyle changes
Lifestyle changes
Be sure to empty your bladder every two to three hours to prevent excessive stress on the urethra. Maintain a healthy weight and quit smoking. Treat constipation and stop straining with bowel movements.
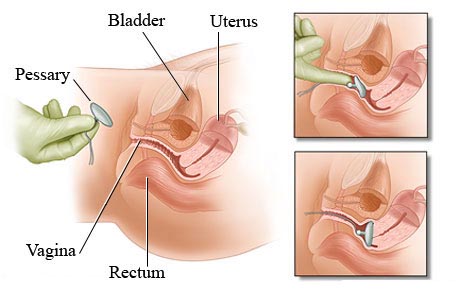
Vaginal pessary
A pessary is a silicone device inserted into the vagina to push the urethra closed and control urine leakage. This allows for normal urination when needed and can be removed at any time.
Pelvic floor physical therapy
Strengthening the muscles that help control continence is a proven, successful treatment for SUI. However, 40 percent of women cannot perform the exercise properly without instruction. It may take two to four months of regular pelvic floor muscle exercises to see improvement. Ask your provider for a referral.
Urethral bulking agents
A substance is injected near the urethra to bulk it so it can help with incontinence when the urethral sphincter weakens. There are different types of bulking agents and the procedure can be performed in the doctor’s office. The procedure is low risk and effects can wear off after several months.
Surgery
There are different types of surgery, including mid-urethral suspensions and urethral slings. Surgery is typically successful and often low risk. Not all women are candidates for surgery. Your provider can discuss these options with you to determine the best course of treatment.
Medication
At this time, there are no medications that help decrease symptoms of SUI. If you have SUI and an overactive bladder (known as mixed incontinence), your provider may prescribe medication to decrease overactive bladder symptoms.
KEY POINTS:
1. Leaking urine is common but not normal.
2. Conservative management with lifestyle changes, pelvic floor strengthening and pessaries are options to improve your symptoms.
3. Lastly, speak to your provider about surgical management of urinary incontinence.
|
Download the Educational PDF